Frequently Asked Questions
- Can I still join the Fall TIPS Collaborative?
- Can we change the fall risk or intervention icons to fit the needs of our hospital?
- Can hospitals not using the Morse Fall Scale implement Fall TIPS?
- Who do I need permission from to use the Fall TIPS tool?
- Do I need permission to use the Morse Fall Scale?
- What care settings/patient populations is the Fall TIPS tool used in?
- What role does the patient care assistant or nursing assistant play in completing the Fall TIPS Posters?
- Is it a HIPPA violation to include the patient’s name on the Fall TIPS poster?
- How can we adapt Fall TIPS for use in covid-19 settings?
- How can I use the Fall TIPS Efficiency Scale (FTES)?
- How can I share my experience with Fall TIPS on the website??
Yes, you can join the collaborative by entering your information here. As a collaborative member you can use the Fall TIPS Toolkit and implement this program at your hospital.
We ask that you do not alter the tool without our permission, since the tool is our property and all of its components are evidence based. We recommend that first, you implement the tool as it is. The language for risk/interventions and icons were rigorously validated with patients and clinical staff. The Fall TIPS tool was iteratively refined until stakeholders felt it was complete and simple to understand.
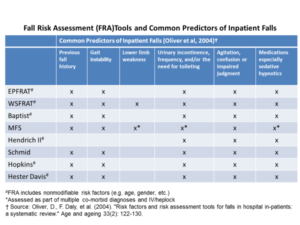
Yes. The Fall TIPS tool is based off the Morse Fall Scale (MFS) because there is the most evidence behind its use in general medical and surgical settings. Studies by Oliver et al show that the MFS is also the only fall risk assessment to address all six common predictors of inpatient falls. The suggested workflow is to complete the fall risk assessment at the bedside with the patients (first in the EHR using your hospital’s fall risk assessment, then using the laminated Fall TIPS poster). This workflow does not burden staff because the fall risk factors align across the most common fall risk assessments and the MFS, as show in the table below:
The Fall TIPS tool is free of charge to use and is available on the resources page of our website. If you require a formal letter, Dr. Patricia Dykes can officially grant permission.
Use of the Morse Fall Scale is free of charge but permission from the author is required. All permissions should be sent to Dr. Morse at Univ of Utah. janice.morse@nurs.utah.edu
While the tool was originally developed and validated for use in general medical/surgical settings, our collaborators are working on adapting the tool for use in psychiatry, rehabilitation, and long-term care settings. The tool is also being used in some intensive care units, emergency departments, and at VA hospitals. If you are interested in implementing in one of these settings, contact us and we would be happy to connect you with one of our collaborators. The tool was not designed for use in pediatric settings, as this requires a completely different fall risk assessment.
Since PCAs do not have access to the Morse Fall Scale documentation in EPIC, they are not supposed to complete the Fall TIPS poster with the patient at the bedside. This is the nurse’s responsibility upon patient admission. However, given the PCAs close relationship with the patient, they have valuable insight regarding updates in the patient’s fall risk status or the best way to assist them. Therefore, the PCAs main role is to notify the nurse when any of these changes occur so that they can be reflected in the Fall TIPS posters. The PCA should also be continuously reinforcing the fall prevention plan with the patient and family members (if present). The PCA can also assist with conducting the Fall TIPS audits, though we recommend that they do so in partnership with the nurse Fall TIPS champion. An important part of the Fall TIPS audits is to provide peer feedback. So, if the poster is not up to date, you should follow up with the nurse responsible. This conversation is vital to identifying any barriers to using Fall TIPS on your units. The PCA may require extra training to feel comfortable in the process, and we have exercises on our website to facilitate this process.
No, it is not as long as the information is used to facilitate care and the patient/family does not object. Many patients/families appreciate seeing the patient’s name on the poster as it shows the patient that is personalized to them and their risk factors. Family members engage the patient in the plan by saying “Look mom it says your name, it’s a personal plan so that you don’t fall!” The tool has been used in over 150 hospitals in our Fall TIPS Collaborative without any issues and is an evidence-based strategy to improve patient safety. However, if having the name on the poster is a concern, sometimes nurses choose to put the patient’s initials on the poster instead of his/her first name.
You can use the same 3-step fall prevention process and maintain the use of champions to conduct audits. The staff may be burdened at this time, making it difficult to complete the audits. Patient engagement may be challenging since covid-19 has placed restrictions on visitors. We are in the process of studying how this pandemic has changed the Fall TIPS workflow. However, nurses have found that engaging patients via unit phones or iPads has been useful. Because evidence suggests that patient and family engagement is key to reducing both falls and fall-related injuries, it is important to find safe ways to do this despite the challenges we now face with covid-19.
The FTES was developed to evaluate nurses’ perceptions of how the use of Fall TIPS effects their workflow efficiency. A copy of the FTES is available on our “Resources” page. We recommend using this tool pre and post Fall TIPS implementation.
You can share your success story with Fall TIPS implementation by emailing our team at PHSFallTIPS@parters.org. Click here for example success stories. We encourage you to include data such as fall rates or fall with injury rates if possible.